Intuitively and not surprisingly, early concerns among members of the wound care community that amputations would likely rise as a result of COVID-19 lockdowns have been validated by multiple sources and published data.1-4
In the outset of the pandemic, many wound care services were deemed non-essential, including those provided in outpatient hospital based wound centers. Patients requiring intensive and regular wound care were suddenly without access to care. The resulting increase in major lower extremity amputations can be attributed to untreated infections and episodes of critical limb ischemia. Critical limb ischemia is a limb threatening decrease in blood flow to the lower extremity, often unrecognized by patients and providers due to its gradual onset from mildly symptomatic peripheral arterial disease to sudden onset of severe symptoms.
One study summed up the impact on diabetic foot ulcer treatment: “the higher risk of amputation observed during COVID-19 lockdown confirms the need for proper and timely management of DFU patients to prevent dramatic outcomes responsible for a reduction of quality of life and increased morbidity and mortality.1
Proper and timely management of any chronic wound is imperative and highlights the importance the Omeza bundle can play in addressing these issues. To further illustrate this concept, a case study is provided:
CASE STUDY
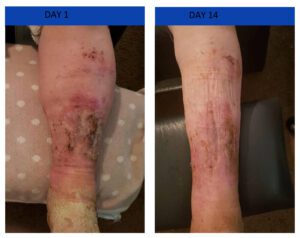
An elderly homebound gentleman with chronic leg ulcers was informed that due to COVID, his visiting physician services would no longer be provided by the company that had been calling on him for over one year. Sedentary and immobile due to vertigo, his edematous legs with open wounds had been dressed with gauze wraps as the primary method of treatment. Upon being informed that home health services were no longer available, the patient’s daughter reached out to a community bulletin board out of desperation, seeking help from anyone who might be of assistance to her father.
The situation was called to the attention of the team at Omeza, who provided guidance and products that resulted in healing of the patient’s leg wounds in approximately 14 days.
The value and benefits of the Omeza products is becoming apparent through clinical results, case studies and our trials. Implementation of wound care protocols using Omeza in both the home and outpatient settings, can be part of an important solution, especially when limited access to essential wound care results in suboptimal outcomes such as infection and amputation.
References:
- Diabetic Foot Problems During the Covid-19 Pandemic in a Tertiary Care Center: The Emergency Among the Emergencies. Caruso P, Longo M, Signoriello S, et al. Diabetes Care. https://doi.org/10.2337/dc20-1347
- Impact of the COVID-19 Lockdown Strategy on Vascular Surgery Practice: More Major Amputations than Usual. Schuivens P, Buijs M, Boonman-de Winter L, et al. Ann Vasc Surg 2020; 69: 74–79 https://doi.org/10.1016/j.avsg.2020.07.025
- Acute Limb Ischemia in Patients with Covid Pneumonia. Bellosta R, Luzzani L, Natalini G, et al. J Vasc Surg. 2020; 72: 1864-72. https://www.jvascsurg.org/article/S0741-5214(20)31080-6/fulltext
- Impact of the Coronavirus Disease 2019 Pandemic on an Academic Vascular Practice and a Multidisciplinary Limb Preservation Program. Lancaster E, Wu B, Iannuzzi J, et al. J Vasc Surg. https://www.jvascsurg.org/article/S0741-5214(20)32018-8/fulltext


